The Gender Pay Gap in Healthcare: Where Do We Stand Now?
As women in medicine, we've been battling the gender pay gap for years.
It often feels like we’re fighting an uphill battle—breaking through glass ceilings, striving to be seen as equals, and constantly pushing for more.
So, where do we stand today?
Examining the current state of the gender pay gap in medicine across states and specialities will enable us, as women in healthcare, to understand exactly where we need to continue pushing for change. Even more, it will enable us to make strides to change the landscape not only for us, but for future women in our fields.
Gender Pay Gap Statistics for Physicians
According to the U.S. Census Bureau, female physicians earned just 72 cents for every dollar male physicians made in 2016.
As residents and fellows, male and female trainees are paid equally based on our postgraduate level. However, on average in practice, female physicians earn nearly $102,000 less than their male counterparts after adjusting for specialty, location, and years of experience. When women were asked whether they believed a gender pay gap existed, 75% said yes—yet only 30% of men agreed.
As mentioned, in training, men and women are compensated the same. So, most of us do not even consider that this may not be the case when we enter practice. But, study after study has shown that the gender pay gap in medicine exists – it’s up to us to figure out why it exists and how to fix it.
Male physicians are reimbursed by Medicare significantly more than female physicians are across all specialties. This was even after adjusting for factors like years of experience, academic rank, clinical volume, and geographic location.
What’s even more striking is that the gender pay gap persists even within the same specialty. When comparing gynecologic and urologic procedures, even when RVUs were matched by procedures in male and female patients, male-specific procedures were compensated at a higher rate 84% of the time.
This isn’t directly about the gender of the physician performing the procedure, but it does highlight the underlying compensation disparities between traditionally male- and female-dominated fields. As such, it is imperative that leaders in our fields and on the RVU committees are aware of and advocates for closing this gap.
In 2023, not a single medical or surgical speciality had equal or higher earnings for female physicians compared to male physicians.
| Specialty | Women Physicians | Men Physicians | % Difference |
|---|---|---|---|
| Allergy & Immunology | $268,000 | $329,000 | 18.50% |
| Anesthesiology | $491,000 | $554,000 | 11.40% |
| Cardiology | $386,000 | $449,00 | 14.00% |
| Colon & Rectal Surgery | $398,802 | $468,984 | 15.00% |
| Dermatology | $501,000 | $591,000 | 15.20% |
| Diagnostic Radiology | $512,000 | $540,000 | 5.20% |
| Emergency Medicine | $373,000 | $386,000 | 3.40% |
| Endocrinology | $269,000 | $324,000 | 17.00% |
| Family Medicine | $239,000 | $286,000 | 16.40% |
| Gastroenterology | $444,511 | $525,931 | 15.50% |
| General Surgery | $460,000 | $479,000 | 4.00% |
| Hematology | $380,847 | $398,113 | 4.30% |
| Internal Medicine | $291,422 | $319,847 | 8.90% |
| Medical Genetics | $240,210 | $249,039 | 3.50% |
| Neurology | $330,000 | $396,000 | 16.70% |
| Nuclear Medicine | $382,000 | $394,000 | 3.00% |
| Obstetrics & Gynecology | $368,000 | $436,000 | 15.60% |
| Oncology | $447,038 | $491,439 | 9.00% |
| Ophthalmology | $459,000 | $549,000 | 16.40% |
| Oral & Maxillofacial Surgery | $395,000 | $568,000 | 30.50% |
| Orthopedic Surgery | $559,221 | $661,801 | 15.50% |
| Otolaryngology | $518,000 | $687,000 | 24.60% |
| Pathology* | $377,000 | $352,000 | -7.10% |
| Pediatrics | $237,168 | $284,286 | 16.60% |
| Plastic Surgery | $389,000 | $438,000 | 11.20% |
| Psychiatry | $313,000 | $344,000 | 9.00% |
| Radiation Oncology | $498,00 | $547,000 | 9.00% |
| Rheumatology | $240,000 | $288,000 | 16.70% |
| Urology | $424,000 | $515,000 | 17.70% |
*The statistic for pathology may have been biased by the proportion of responses (74% women), and the fact that it includes dermatopathology, a subspeciality that is higher earning than pathology alone. Many dermatology-trained dermatopathologists practice both pathology and dermatology concurrently.
Click on the specialty to view source of statistics. Statistics were unavailable for Cardiothoracic Surgery, Interventional Radiology, Neurosurgery, Physical Medicine and Rehabilitation, and Vascular Surgery.
We are on the right track, though. In 2023, 12 specialties had narrowed their gender pay gap to less than 10%. That’s a significant improvement compared to only 2 specialties achieving this in 2022.
As the number of women in medicine continues to grow, these numbers suggest we are moving in the right direction.
However, we still have our work cut out for us. It is up to us as women in medicine to share awareness, insight, and experience to close the gap for ourselves and those who will come after us.
Gender Differences in Pay by State
Throughout the United States, studies have shown that female physicians earn about 15-20% less than their male counterparts. This gap varies significantly by state, specialty, setting (urban vs. rural), and local cost of living. While this is not something that should change where we choose to practice, it is important to be aware of when negotiating our contracts.
Some examples of reported disparities include the following:
California: Female physicians earn approximately 87% of what male physicians make.
New York: Female physicians earn approximately 86% of what male physicians make.
Texas: Female physicians earn about 79% of what male physicians make.
Florida: Female physicians earn approximately 78% of what male physicians make.
Massachusetts: Female physicians earn approximately 92% of what male physicians make.
In addition, a study examining differences in Medicare reimbursement by gender by state found that in all states, men were reimbursed more and had a greater number of services billed for than women.
These differences were most pronounced in procedural specialties including ophthalmology, dermatology, cardiology, and otolaryngology.
The states with the highest gender differences in Medicare reimbursement were as follows:
Florida: $66,000.63
Delaware: $65,140.93
Alabama: $61,925.30
Mississippi: $61,845.83
Louisiana: $55,835.57
The states with the lowest gender differences in mean reimbursement were as follows:
Minnesota: $13,751.97
Wyoming: $14,749.28
Vermont: $16,990.12
Alaska: $17,742.21
Wisconsin: $21,147.15
Again, highlighting these disparities is important for us as women in medicine to be aware of as it is a feasible target for intervention – ensuring that we code appropriately for all services provided may help to close the gender pay gap.
Source: medRxiv
Gender Differences in Pay by Practice Setting
Female physicians continue to face challenges when it comes to equal compensation, not just from employers, but from other sectors as well.
For example, a 2022 study found that men received higher and more frequent payments from the industry compared to women – only 1 of the 15 companies included in the study had a female CEO.
It is important that leaders of these companies as well as those of us working with industry advocate to even the compensation rates. We are no less qualified to be key opinion leaders in our fields, so we should not be treated like we are.
This trend also plays out in academia, where female physicians are less likely to hold leadership roles and tend to have lower H-index scores. Unfortunately, based on the discussion above this is not a surprise – it is, however, disappointing and a place for us to work to change.
Gender Differences in Pay for Other Healthcare Professionals
We've talked a lot about the pay gaps for women physicians, but it's important to remember that other female healthcare providers, like nurses and Advanced Practice Providers (APPs), also face similar issues.
Even though some of these fields are predominantly composed of women, the pay gap between men and women still exists, and it's something we need to keep addressing. We as women in medicine need to support each other in our fight for equality.
Gender Differences in Pay for Nurses by Position/Degree
| Position | Women | Men |
|---|---|---|
| Advanced Practice Registered Nurse | $104,000 | $120,000 |
| Registered Nurse | $72,700 | $80,000 |
| Licensed Practical Nurse | $45,000 | $45,000 |
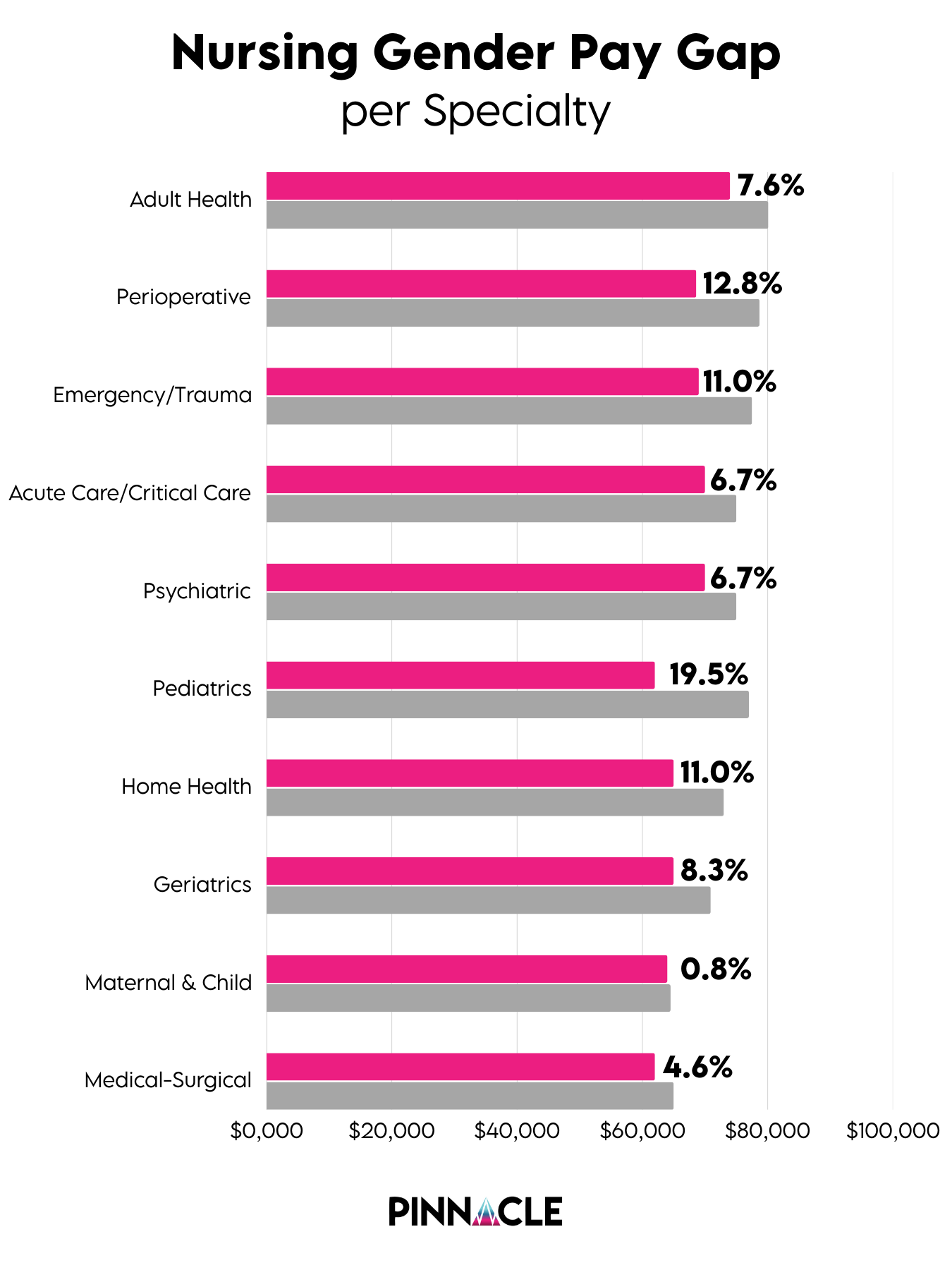
Gender Differences in Pay for Nurses by Specialty
| Specialty | Women | Men |
|---|---|---|
| Adult Health | $74,000 | $80,100 |
| Perioperative | $68,600 | $78,700 |
| Emergency/Trauma | $69,000 | $77,500 |
| Acute Care/Critical Care | $70,000 | $75,000 |
| Psychiatric | $70,000 | $75,000 |
| Pediatrics | $62,000 | $77,000 |
| Home Health | $65,000 | $73,000 |
| Geriatrics | $65,000 | $70,900 |
| Maternal & Child | $64,000 | $64,500 |
| Medical-Surgical | $62,000 | $65,000 |
Statistics for Advanced Practice Providers
| Profession | Women | Men |
|---|---|---|
| Nurse Anesthetists | $180,790 | $199,981 |
| Nurse Practitioners | $109,873 | $123,014 |
| Physician Assistant | $101,000 | $112,500 |
What’s Driving the Pay Gap in Medicine?
There’s no one reason why the gender pay gap exists in medicine. As mentioned above, the studies comparing the gender pay gap controlled for expected differences like specialty, location, and years of experience. So, what is causing the gap? And even more importantly, what can we do about it?
First, many specialties with a higher proportion of women tend to be lower-paying. Fields like Pediatrics, Child & Adolescent Psychiatry, and Geriatric Medicine, for example, often have lower salaries compared to specialties like Gastroenterology or Orthopedics.
We also know that women are underrepresented in high-compensation specialties, which can have a big impact on earnings over time. Even recently, women have been found to be underrepresented among residents entering into high-compensation specialties.
Whether that is due to lack of mentorship or other issues, those of us in high-compensating specialties should remember that whether in academia, private practice, or other ventures, we can encourage students and residents to chase their goals.
The next topic to consider is the differences we face if we have kids.
In a study published in JAMA Internal Medicine found that, after having children, women in dual-physician households typically work 11 hours less per week than their male counterparts with children – or even compared to other women without kids.
This drop in hours can translate into fewer RVUs (Relative Value Units), which directly impacts pay.
Women face this pressure to choose – doctor or mom. But why can’t we have both? And, why is there a difference in how many hours men with children and women with children work? We need to remember as women in medicine that times are changing and we CAN have it all.
How to navigate having children as female physicians historically has felt like a taboo subject. But, it doesn’t have to be. Even amongst us at Pinnacle, many of our faculty have kids and thrive as moms and physicians. Leaning on each other for advice and using our platforms to talk about how we make it work are ways to help others undergoing the same struggles.
In addition to differences in work hours and specialty choice, there are other factors that have been cited as contributing to the gap, like differences in negotiation skills and access to powerful networks. But is this really the case? It shouldn’t be. Being a woman does not make us any less able to negotiate effectively. And, I hope in 5, 10, and 15 years, this isn’t even a thought. The only way to change that stereotype, however, is by our own actions.
These challenges are not unique to any one woman or one field of work—they are systemic issues that we need to address collectively. We need more transparency regarding salaries and less stigma surrounding discussion. It is okay, even encouraged, to discuss our salaries amongst each other. Open discussion, mentorship, and supporting each other is how we can take control and fight for our equality.
Senior physicians, APPs, nurses, and other leaders, male and female, must take a role in changing the culture at academic institutions, private practices, HMOs, and even smaller organizations where pay inequality is occurring in order to bring about change. Just as important is our role as women in medicine to advocate for ourselves and those around us.
Conclusion
While the gender pay gap in medicine remains a persistent challenge, the growing awareness of these disparities is a step in the right direction. With resources like Pinnacle to connect us, we can work together to change the landscape of being a woman in medicine.
As more women enter the field and continue to push for equality, we are starting to see positive changes – though there's still plenty of work ahead.
By continuing to advocate for fair compensation, pushing for leadership opportunities, and supporting one another, we can help close the gap for the next generation of women in medicine.